Anatomy and Physiology
5 Skin
 ʻAʻohe like o ka ʻili
ʻAʻohe like o ka ʻili
The skin is not alike
ʻŌlelo Noʻeau, compiled by Mary Kawena Pukui, #172
Introduction
![]() Chapter Learning Outcomes
Chapter Learning Outcomes
- Describe the components of the integumentary system and how they contribute to homeostasis.
- Describe the skin, including the functions of its cell types and layers
- Describe the anatomy and physiology of the accessory structures of the skin
- Discuss skin injuries and disorders and address healing and treatments
 |
 |
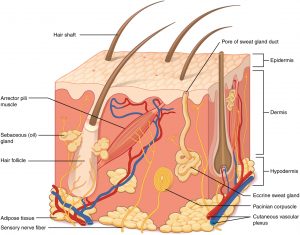
Do you remember going to the beach and playing in the water on a sunny afternoon? Have you ever wondered how your body protects you from the sun or from getting wet? Although you might think of organs as your internal organs such as your heart, lungs, and liver, your skin is also an important organ. In fact, your skin is the body’s largest organ and makes up about 7 to 8% of your total body weight. Your skin makes up the majority of the larger , which includes , nails, oil and sweat glands, and sensory receptors. One of the primary functions of your integumentary system is to protect the inside of your body from the external environment, but it is also important in maintaining homeostasis in body temperature and your blood circulation. The integumentary system also has important sensory functions, which is why you’re able to feel pressure, temperature, pain, and other senses that you perceive through touching your environment.
Skin Structure
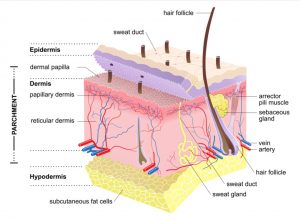
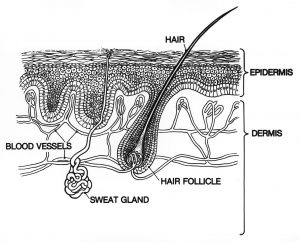
Fig. 5.1: Layers and Accessory Structures of the Skin
5.1 Epidermis
![]() 5.1 Learning Outcomes
5.1 Learning Outcomes
- Describe the layers of the epidermis and their characteristics
- Describe the diseases and factors that affect the epidermis
The is the outermost layer of the skin and is exposed to the outside environment. Most of the cells of the epidermis are s arranged in a stratified squamous epithelial layer, but there are also tactile epithelial cells, intraepidermal macrophages, and s embedded throughout the epidermis. Tactile epithelial cells (s) are sensory receptors for touch, sending signals via sensory neurons to the brain. Intraepidermal macrophages (s) destroy invading microbes to prevent them from breaking through the skin and entering the body where they could spread.
As cells divide in the deepest layer of the epidermis known as the (stratum germinativum). As they divide they push up previous cells into sublayers and start to develop distinct characteristics as they enter each layer. You will also see that each sublayer serves a distinct function in terms of protection. Let’s examine the five sublayers of the epidermis and see where we find each of the epidermal cell types.
 |
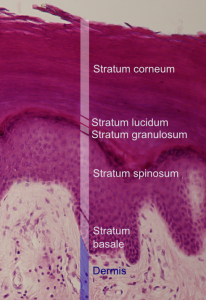 |
| Epidermis: Drawing of Skin Layers | Epidermis: Histological Slide of Skin Layers |
Fig. 5.2: Drawing and a histological section showing all five sublayers of the epidermis
Stratum Corneum
The is the outermost layer of the epidermis and the epidermal sublayer exposed to the outside environment.
As keratinocytes divide and grow toward the outside environment, they produce and accumulate a hydrophobic protein called . Keratin (Grk. keras “horn”), is a fibrous protein that also is the main constituent of hair and nails. Keratin is a protein that is well conserved across animal species and we see that keratin also is the major component of hooves, feathers, and horns in other animals. It protects from cuts, toxins, burns, and microbes. The increased keratinization (cornification) of the cells in this layer gives it its name, and as cells form and accumulate keratin filaments, they start to dehydrate and become dry due to the hydrophobic nature of keratin.
There are usually 15 to 30 layers of cells in the stratum corneum. This dry, dead layer helps prevent the penetration of microbes, the dehydration of underlying tissues, and provides mechanical protection against abrasion for the more delicate, underlying layers. In addition, exocrine gland secretions, such as sweat, which contains demicidin, prevent the growth of microorganisms. Cells in this layer are shed periodically and are replaced by cells pushed up from the (or in the case of the palms and soles of feet). The entire layer is replaced in about 4 weeks. Cosmetic procedures, such as microdermabrasion, help remove some of the dry, upper layers and aim to keep the skin looking “fresh” and healthy.
Stratum Lucidum
If present, the stratum lucidum is located just below and deep to the stratum corneum. The stratum lucidum is named after its translucent appearance when viewed under a histological microscope slide. The keratinocytes in the stratum lucidum are dead and flattened and densely packed with , a clear lipid-rich protein that gives these cells their transparent “lucid” appearance and provides a hydrophobic barrier. The stratum lucidum is a relatively thin sublayer of cells and is only found in certain regions of the body. The stratum lucidum is present only in thick skin, which has all five epidermal sublayers and is located exclusively in the palms, soles, and digits.
Stratum Granulosum
The stratum granulosum is named due to the appearance of granules that form in keratinocytes as they are pushed from the . The stratum granulosum is mostly composed of three to five layers of keratinocytes that flatten and thicken their membranes and produce large amounts of the proteins keratin and , which accumulate as granules within the cells. These two proteins make up the bulk of the keratinocyte mass in the stratum granulosum and give the layer its grainy appearance. The proteins in these granules will be used in further keratinization of the keratinocytes as they are pushed up into the superficial layers of the epidermis. Additionally, the nucleus and other cell organelles of keratinocytes start to disintegrate as the cells transition through the stratum granulosum. This disintegration of organelles causes keratinocytes to die in the stratum granulosum, leaving behind the keratin, keratohyalin, and cell membranes that will form the stratum lucidum, the stratum corneum, and the accessory structures of hair and nails.
Stratum Spinosum
As the name suggests, the stratum spinosum is named after its spiny appearance after being viewed in a microscope. This spiny appearance is caused by s and cytoskeletal components that join keratinocytes to each other in this layer and the chemical processes that occur during the staining procedures done in making a microscope slide. Unstained epidermis samples do not exhibit this characteristic appearance. The stratum spinosum is composed of eight to 10 layers of keratinocytes that are formed from cell division in the stratum basale, which pushes keratinocytes up into the stratum spinosum. The stratum spinosum is also noticeable in that intraepidermal macrophages (Langerhans cells) tend to be present in this layer, although they can be found throughout other layers of the epidermis (but rarely in the stratum corneum). Intraepidermal macrophages are macrophages that help carry out the skin’s protective functions by engulfing bacteria, foreign particles, damaged and cancer cells that occur in this layer.
Stratum Basale
The stratum basale is the deepest epidermal layer and is also called the stratum germinativum, as it contains s that actively divide and regenerate the layers of the skin. The stratum basale also forms the “base” of the epidermis and attaches it to the basal lamina, which forms a transitional layer between the epidermis and the . The cells in the stratum basale bond to the dermis via intertwining collagen fibers, referred to as the basement membrane.
The stratum basale is a single layer of cells primarily made of basal cells (basal keratinocytes). A basal cell is a special type of stem cell that can regenerate more basal cells and differentiate and develop into keratinocytes of the epidermis. As basal cells divide, they push up layers of cells which eventually form the five layers of the epidermis. All keratinocytes are produced from this single layer of cells, which are constantly going through mitosis to produce new cells. Recall that mitosis is where a cell duplicates its organelles and DNA into two daughter cells. As new cells are formed, the existing cells are pushed superficially away from the stratum basale and toward the external environment of the body. Two other cell types are found dispersed among the basal cells in the stratum basale. Tactile epithelial cells (Merkel cells), function as sensory receptors and stimulate sensory nerves that result in your sense of touch. These cells are especially abundant on the surfaces of the hands and feet, thus making those surfaces very sensitive to your sense of touch. Separating the epidermis from the connective tissue of the dermis are hemidesmosomes.
![]() Clinical Application
Clinical Application
 Calluses
Calluses
When you start learning how to play the ukulele, you experience the formation of es due to the repetitive injury of the cells in the epidermis. Although these cells are dead, they are resistant to mechanical damage due to the presence of keratin. This occurs because the basal stem cells in the stratum basale are triggered to divide more often to increase the thickness of the skin at the point of abrasion to protect the rest of the body from further damage. These calluses, although uncomfortable, are your “friends” because they are preventing further harm to the skin. Over time, the calluses will shrink on their own, so there is no need to do too much about it. The best thing to do to decrease the pain when playing ukulele is to keep playing and leave the calluses alone! Now choose the ukulele that best fits your body type and enjoy the music!

Fig. 5.3. A picture showing the relative size and scale length of the ukulele family of instruments.
Melanocytes and Skin Color
Melanocytes are cells that are abundant in the stratum basale, and they produce a chemical called that is important in the protective functions of the skin.
Melanin is a pigment that works as a natural protective sun umbrella or sunscreen in keratinocytes. This pigment is produced in response to exposure to ultraviolet light. Melanin occurs in two primary forms in the human body. Eumelanin is a dark brown or black pigment and pheomelanin is a reddish pigment. These natural pigments play a large role in determining the color and tone of your skin. In general, people with darker skin tones produce a higher concentration of melanin than individuals with paler skin. Carotene is another category of chemical pigment that can affect the color and tone of your skin, but instead of being produced by your body, it is obtained from your diet. Sources of carotene include carrots, sweet potatoes, squashes, and pumpkins.

Fig. 5.4: Photograph of UH students with a spectrum of skin tones
People with have melanocytes, but their melanocytes are unable to produce melanin due to a deficiency of tyrosinase, an enzyme that plays a role in melanin biosynthesis. As a result, their skin and hair appear pale or white. Melanin is also responsible for eye color, which is why people with albinism often have irises that are blue or red (from the blood vessels).

Fig. 5.5: Photograph of a child with albinism
is another condition related to melanocytes. Someone with vitiligo has patches of lighter skin compared to the rest of their body, and this is due to the lack of melanin in the affected areas. Although scientists and doctors are still researching what exactly triggers vitiligo, most theories suggest that the immune system is involved. Normally, your immune system should protect your body against foreign substances and disease-causing pathogens, but in vitiligo, it is widely thought that the immune system is attacking melanocytes, causing them to die and resulting in a lack of color and pigment in the affected areas.

Fig. 5.6: Photograph of a man with vitiligo Individuals with vitiligo experience depigmentation that results in lighter colored patches of skin. The condition is especially noticeable on darker skin.
But how does melanin get from the melanocytes to the superficial layers of keratinocytes? Although melanocytes have the majority of their cell body in the stratum basale, they have projections that reach toward the outer superficial layers of the skin. Melanocytes transfer melanin to keratinocytes by secreting s, which are cellular vesicles that contain melanin and carry melanin over to keratinocytes, which pick up the pigment that collects above the keratinocyte nucleus, thus shielding its DNA from sun damage from the outside environment.
Ultraviolet Light
As you are swimming and playing at the beach, you can feel the sun’s energy on your skin. Have you ever wondered why the sun damages your DNA, and why is it important that melanocytes secrete melanin to protect your skin and other cells? Light is actually a form of radiation, and the sun emits a wide spectrum of radiation that includes the visible light we see and other types of invisible radiation. Ultraviolet (UV) light is a form of radiation that carries more energy than the visible light you can see. The high amounts of energy carried in UV light can also break the chemical bonds that hold the molecules of your cells and body together. When a UV photon (a particle that carries energy in the form of light) strikes a DNA molecule, it can break the bonds that maintain the structure of DNA or the bonds that make up the base pairs that encode the information contained within DNA. The melanin produced by melanocytes can protect the nuclei of your cells by absorbing the energy carried by UV light, thus preventing those high-energy photons from damaging DNA and cells located beneath the melanin. Your melanocytes are also sensitive to UV light, and they respond to UV exposure by increasing their production of melanin. This is why you tan when you spend time outdoors or actively try to tan and sunbathe — your melanocytes are trying to protect you from the increased UV radiation by producing more melanin.
Commercially-bought sunscreens have chemical compounds which are intended to absorb UV light and protect your cells and tissues. Dermatologists often recommend sunscreens to people who live in areas with a lot of yearly sunlight (such as Hawaiʻi) or spend a lot of time outdoors to protect them against the increased exposure to UV light.

Fig. 5.7: UV Light Demonstration of the effect of sunscreen. The man’s face has sunscreen on his right side only. The left image is a regular photograph of his face; the right image is of reflected UV light. The side of the face with sunscreen is darker because the sunscreen absorbs the UV light.
Skin Cancers
Remember that DNA contains all the instructions to make every single one of your cells, how to undergo mitosis and produce more cells, and make all the proteins and molecules that keep the cells alive. Although UV radiation isn’t the only potential cause of DNA damage in your body, it is one of the major causes of skin cancer, as the skin is your body’s first line of defense against UV radiation.
If the basal cells in the stratum basale accumulate enough DNA damage to grow abnormally and rapidly, it can result in basal cell carcinoma (BCC), a type of skin cancer. BCC is actually the most common form of skin cancer and can potentially develop anywhere on the skin. BCC often appears as a raised patch or bump, since the rapidly dividing cancerous cells in the stratum basale will form a mass that pushes up the outer layers of the epidermis. Although BCC is a type of cancer and sounds potentially scary and threatening, the good news is that BCC growths are easily removed by cutting out the cancerous tissue and allowing the skin to heal as it rarely requires additional chemotherapy. People rarely die from BCC, and if detected early, it can be treated well before cancerous cells can spread to the rest of the body.

Fig. 5.8:
is another type of skin cancer, but it develops from melanocytes that have accumulated enough DNA damage and mutations. Surprisingly, melanin does not provide such effective protection to the melanocytes themselves. Melanoma is also remarkable in that it displays distinct characteristics and appearances compared to other skin cancers (Figure: ABCDEs of melanoma). Unlike basal cell carcinoma, melanoma has a higher chance of spreading beyond the skin and invading other parts of the body. This invasive form is called malignant melanoma and is difficult to treat as it can spread throughout the body to the point that it is impossible to remove all the cancerous melanoma cells and tumors. This is why melanoma is the deadliest form of skin cancer, and why early detection is important to catch melanoma before it spreads throughout the body.
|
|
|
|
|
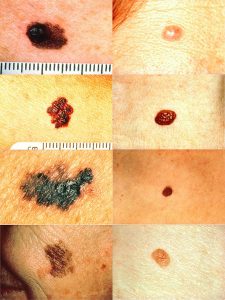
Fig. 5.9: ABCDEs of melanoma (a) Chart (b) ABCD rule illustration: On the left side from top to bottom: melanomas showing (A) Asymmetry, (B) a border that is uneven, ragged, or notched, (C) coloring of different shades of brown, black, or tan and (D) diameter that had changed in size. The normal moles on the right side do not have abnormal characteristics (no asymmetry, even border, even color, no change in diameter).
Melanomas are often mistaken as moles, or nevus (plural: nevi), which is a general term describing a rounded mark on the skin. Moles are often dark due to them forming from the increased growth of melanocytes in that area. Unlike melanomas, the growth of melanocytes in moles is non-cancerous and benign, and not life-threatening. However, moles can infrequently develop into melanomas if a melanocyte in a nevus becomes cancerous, which is why it is important to be aware of rapid changes in moles that show symptoms such as the ABCDEs of melanoma.
Vitamin D3
Although UV light can potentially damage DNA and other molecules in your cells and tissues, it also plays an important beneficial role in the homeostasis of your body. The energy contained within UV light can also be used by your body to break the chemical bonds needed to make vitamin D3 (cholecalciferol) in the epidermis. Vitamin D is a group of hormones that includes vitamin D3 and is generally important in maintaining homeostasis in your blood calcium levels and the integrity and structure of your skeleton. A lack of also can increase your risk for certain types of cancers, including breast cancer and colon cancer. Your skin’s production of vitamin D is also affected by the amount of melanin in your skin. Although melanin absorbs UV light and protects DNA, it also prevents UV light from breaking the bonds needed to convert chemicals into vitamin D3. This is why medical professionals may monitor levels of vitamin D in people who have increased melanin and darker skin tones to ensure that they have enough vitamin D and are not at risk of diseases caused by vitamin D deficiency.
Differences between Thick and Thin Skin
Recall that the epidermis is composed of many strata (layers) of cells. Our skin is categorized as either thick or thin skin, according to the number of the epidermal layers. Found on the palms of the hands and soles of the feet, the thick skin has all five layers and sweat glands. This skin doesn’t have s or s. On the other hand, thin skin has only four layers, with no stratum lucidum, and has sebaceous and sweat glands and hair follicles.

Fig. 5.10 Skin: Thick and thin skin cross sections
5.2 Dermis
![]() 5.2 Learning Outcome
5.2 Learning Outcome
- Describe the layers and composition of dermis
The dermis is located right underneath and immediately deep into the epidermis and consists of two main sublayers: the , and the . The dermis is made up of connective tissues that form a dense network of protein fibers such as elastin and collagenous fibers. The dermis is rich in fibroblasts, which produce large quantities of matrix and protein fibers that make up much of the structure of the dermis. The dermis also provides a scaffold that gives structure for a network of blood and lymph vessels. These vessels are not only important in delivering oxygen and nutrients to your skin, but also in carrying heat and regulating temperature homeostasis, and also in regulating fluid and blood volume homeostasis in your body.
The dermis also has many sensory receptors and nerves that transmit signals that cause your overall general sense of touch. The dermis also contains accessory structures such as hair follicles and sweat glands.
Papillary Layer
The papillary layer is the superficial sublayer of the dermis and is made of areolar connective tissue that contains a loose mesh of collagen and . The papillary layer is named after its plethora of finger-like projections, known as dermal papillae (singular = ). Dermal papillae also protrude and project into the stratum basale of the epidermis, causing a wave-like border between the epidermal stratum basale and the dermis. Dermal papillae increase the strength of the connection between the epidermis and dermis by increasing the surface area and cellular connections between the epidermal and dermal layers. The greater the folding in this region, the greater the surface area and the stronger the connections.
The structure of the papillary layer also forms structures called friction ridges, which form the basis and shape of your fingerprints. In a growing fetus, fingerprints form where the cells of the stratum basale meet the papillae of the underlying dermal papillary layer, resulting in the formation of the ridges on your fingers that you recognize as fingerprints. Fingerprints are unique to each individual and are used for forensic analyses because the patterns do not change as you grow and age.
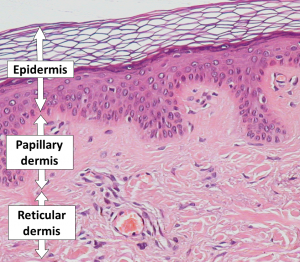
Fig. 5.11: Histological slide showing layers of the dermis, including the interface between the dermis and epidermis
 |
 |
| Fingerprint – Central Pocket Loop Whorl with a spiral center | The friction ridges on a finger |
Fig. 5.12: Fingerprints
The papillary layer contains numerous fibroblasts, a few fat cells (adipocytes), and an abundance of small blood vessels. In addition, the papillary layer contains phagocytes, which are immune cells that help defend the body and fight against bacteria or other infections that have breached the skin. The papillary layer also contains lymphatic capillaries, nerve fibers, and specialized receptor cells called tactile corpuscles (s) that are part of your sense of touch.
Reticular Layer
The reticular layer of the dermis is located just below the papillary layer and is made up of a much thicker layer of dense, irregular connective tissue. This dermis has an extensive network of blood and lymph vessels and nerves. The reticular layer is named after its reticulated (net-like) woven meshwork of protein fibers. Elastin fibers provide stretch and durability to the skin — these fibers allow your skin to move and distort, but also help your skin move back into place. Collagen fibers provide structure and further tensile strength to the dermis, and gram-for-gram, are stronger than steel cables. These strands of collagen extend across both the papillary layer and the .
The arrangement of collagen fibers in the dermis determines cleavage lines (Langer’s lines) in your skin, which follow the direction of collagen fibers in your dermis. Cleavage lines also run perpendicular to muscle fibers below your skin. Surgeons consider the arrangement of cleavage lines when operating and deciding where to cut and make an incision. Making incisions parallel to cleavage lines results in less ring than if a surgeon were to cut across and perpendicular to the lines.
Ultraviolet A wavelengths of UV light can penetrate the skin past the epidermis and into the dermis. Remember that UV light carries energy that can break chemical bonds, and molecules in your body are held together with chemical bonds to keep their structure. UV light can damage more than DNA — it can also damage and break chemical bonds in collagen and elastin protein fibers, which is why people who are exposed to high levels of UV light experience photoaging, which describes changes in the skin from its original undamaged quality. People who experience photoaging have a loss in skin turgor, which refers to the overall elasticity and structure of your skin, which can also lead to wrinkling and thinning of the layers of the skin.
Collagen also attracts and binds water to keep the skin hydrated. Cosmetic collagen injections and tretinoin (Retin-A) creams help restore skin turgor, by either injecting additional collagen or stimulating the body’s blood flow and collagen production. One should always consult the opinions of your dermatologist or doctor before such treatments.
Tattoos, including Hawaiian kākau, are performed by delivering pigments into the dermal layer of the skin via needles or other sharp instruments. Tattoo colors and pigments must be delivered past the epidermal layer, otherwise, they will be eventually pushed up into layers of keratinocytes and shed as part of the stratum corneum. If you have a tattoo, you may have noticed that over time the tattoo appears less intense and lighter compared to when you first received it. The design that remains are the pigments that stayed in the dermis.
![]() Cultural Connection
Cultural Connection
Kākau
Pāʻele kū lani.
The chiefy blackening.
‘Ōlelo No’eau, Compiled by Mary Kawena Pukui, #2565
This expression, used in chants and songs, refers to the tattooing of Kahekili II, full name Kahekilinuiʻahumanu, (c. 1737–1794) , ruler of Maui. Because he was named for the god of thunder, who was believed to be black on one side of his body, Kahekili had himself tattooed on one side from head to foot.
The tradition of applying tattoos began in the Polynesian islands over 2000 years ago and has deep roots among the indigenous peoples of Polynesia. As the tradition spread, each island culture brought its own style. For example, moko is a traditional tattoo of the Māori people of New Zealand. The Hawaiian tattoo art known as kākau and kā uhi, serves not only as ornamentation and sign of distinction but to guard the health and spiritual well-being. The designs are applied by specially trained kā uhi practitioner using pigment to the skin with a needle made from bone. To learn more about the history and pictures of Polynesian tattoos, go to the PBS Hawai’i site on Skin Stories. Also see ʻŌiwi TV program Nā Loea: The Masters | Keone Nunes: Ancestral Ink linked below.
 |
 |
| Jason Momoa with kākau on his arm | Hon Nanaia Mahuta – Labour candidate for Hauraki-Waikato in the 2020 New Zealand Election, with Tā Moko |
 |
 |
| Samoan Malu Female Tattoo | Whang-od, a mambabatok of the Kalinga in the Philippines, performing a traditional batek tattoo with a mallet and hafted needles |
Fig. 5.13: Traditional Pasifika and Philippines Tattoo Arts
Subcutaneous Layer
The subcutaneous (“sub-”= “below” + “-cutaneous”= “skin”) layer, also called the hypodermis (“hypo-”= below + “-dermis”= skin) is not a part of the skin but is attached to the dermis and in some regions is difficult to distinguish from the dermis. Think about what is beneath your skin. Muscles and bones, right? The subcutaneous layer connects your skin to the connective tissue that surrounds your muscles and bones. That connective tissue is called the fascia. Going from superficial to deep, you have skin, subcutaneous layer, fascia, muscle, and bone. [Figure: Subcutaneous Layer (cross-section showing skin, subcutaneous layer, fascia, muscle, ] The subcutaneous layer contains blood vessels that bring nutrients to, and remove waste from, the skin. There are also pressure-sensitive nerve endings called lamellated () corpuscles. The tissue in the subcutaneous layer, also called subQ layer, is areolar and fat (adipose) tissues. You may have heard of subcutaneous fat. This is the place. This layer of subQ fat thins with age and contributes to the look of older skin as well as increased risk of injury and less insulation against cold weather. Imagine the delicate skin on the back of the hand of your tutu (grandparent in Hawaiian).
![]() Deep Dive
Deep Dive
In Hawai‘i, we have many plants that are used for natural health and healing of the skin and hair. For example, noni, which has antioxidants, nutrients, and essential fatty acids is used by some people to keep their skin healthy and to help recover from sunburns. Explore, at our farmer’s market or ask family and friends, to learn more about local plants and foods that nourish the skin and hair. Go to PubMed.gov and search some of these items to see the scientific studies that describe many of the constituents of these plants and how they work.
 |
 |
| Young Noni Plant | Noni Fruit (Morinda citrifolia) |
5.3 Accessory Structures of the Skin
![]() 5.3 Learning Outcome
5.3 Learning Outcome
- Describe the structures and functions of hair, nails, and glands
Hair
You may think a lot of things about your hair, but did you ever imagine it is providing you with protection? On your head, the hair is shielding your skin from the sun. The hairs inside your nose and ears, along with eyebrows and eyelashes, can trap things like dust and dirt so are providing a defense. Your eyebrows slow down the flow of sweat into your eyes. With their sensory receptors in the root, they even provide sensory information about touch. Hair, also called pili, is found everywhere except the palms of your hands and soles of your feet.
Hair is mostly made of dead, keratinized cells, growing out of the epidermis. The is the part you see, with most of it extending beyond the skin surface. The is below the surface of the skin and goes down into the dermis. [Insert Figure of Hair (section through skin showing a hair and view of individual hair showing layers)] The lower region of the hair root is the hair follicle, with its deepest portion being the . Inside the bulb is the papilla of the hair with nerve endings as well as blood vessels to provide nourishment to the living cells here called the . The matrix cells produce replacement hairs when the old hair is shed.
The root and shaft are made of three layers, from superficial to deep: , , and . The cuticle is the outer layer and is made of keratinized cells that are very hard. Deep into that, the keratinized cells form a layer that is not as hard and that is the cortex. The cortex provides the structure that determines if the hair is curly or straight. The medulla is the central region and is sometimes not present in thin hair. This is the region that has different pigments that dictate hair color. There are more pigment granules in darker hair, fewer for lighter hair, and very few in hair that is gray.
When you get “chicken skin” or “goosebumps” on your skin because you are suddenly frightened or very cold, this is due to (raise + hair), a bundle of smooth muscle cells beside the hair follicle.
 |
 |
| Frightened Cat | Chicken Skin |
Fig. 5.14 Chicken skin
The muscle pulls the hair to make the hair stand on end. You may have seen this on the back of a frightened cat. But why does the cat do this and why do we have this? If we go back far enough in time, when our ancestors were covered with fur, imagine the advantage if another creature jumped out at us. All our fur would stand up and suddenly we would appear larger and hopefully scarier. Regarding the cold, that fur standing on end, rather than in the resting position lying flat along the skin, provides an air pocket to trap warm body heat and hold it close to us.
As you have noticed, thankfully your hair is replaced after it is shed. This is because of the three stages of the hair growth cycle. Hair becomes longer during the growth stage, when the matrix cells of the hair bulb multiply, pushing the existing cells up. On their way toward the top, these cells become keratinized and are no longer living cells. A single scalp hair can be in the growth stage for two to six years and around 85% of your hair is in this phase at any given time. Even though the parts of those hairs that you see are nonliving tissue, the root is quite alive. Next, during the regression stage, hair quits growing because the matrix cell division stops, causing the hair follicle to shrink. That phase lasts two to three weeks. The hair falls out during the resting stage and then a new growth cycle begins in around three months. Hair loss happens at a wide range of rates and for a variety of circumstances. Normally, you will lose 70-100 hairs each day. It is true that extreme emotional stress can, indeed, make you lose more hair. What you eat also affects your hair. A severe reduction in calories or protein can cause hair to fall out.
We have been referring to hair as a single entity, but there are three types of hairs. A fetus is covered with soft, fine hair called lanugo. Perhaps you have heard the word, lanolin, which refers to the oil in sheep wool. The word lanugo has the root, lana, which is Latin for wool. The lanugo is not thick and full like wool, but it is very soft. Before a baby is born, the hair of the scalp, eyelashes, and eyebrows turn into terminal hairs which are likely the type of hair you have been imagining throughout this chapter. The hair everywhere else is called vellus hair. At puberty, hormones change the vellus hairs of the armpits (axillae) and pubic regions to terminal hairs. In males, the face and body will also have terminal hairs in assorted areas resulting in things such as beards and chest hair. Females have terminal hair on the face and body regions but to a much lesser degree than males, and with large variation between individuals.
![]() Clinical Application
Clinical Application
Chemotherapy
Remember the matrix cells and how their division brought about hair growth? Some of the chemicals used to treat cancer are trying to stop cells, such as tumor cells, from multiplying. Since these chemicals target cells that in particular are dividing rapidly, they disrupt the matrix cell division, and thus a person having chemotherapy usually experiences hair loss. The matrix cells that are in hairs in the resting stage of the hair growth cycle are not destroyed by chemotherapy because they are not rapidly dividing. Ultimately, those matrix cells replace the follicles that were lost and the new hair grows.
Nails
The is a specialized structure of the epidermis that is found near the tips of our fingers and toes. The is a hard layer formed on the nail bed and protects the fingers and toes as they are parts of the body that experience exposure and mechanical stress.

Fig. 5.15 Nail Anatomy
In addition to protection, the nail body forms a back-support for picking up small objects with the fingers. The nail body forms at the , which has a nail matrix of proliferating cells from the stratum basale that enables the nail to grow continuously. The nail is composed of densely packed dead keratinocytes. The lateral overlaps the nail on the sides, helping to anchor the nail body. The nail fold that meets the proximal end of the nail body forms the , also called the (above + nail). The nail bed is rich in blood vessels, making it appear pink, except at the base, where a thick layer of epithelium over the nail matrix forms a crescent-shaped region called the (little moon). The area beneath the free edge of the nail, furthest from the cuticle, is called the (below + nail). It consists of a thickened layer of stratum corneum.
![]() Clinical Application
Clinical Application
Long-term exposure to warmth and moisture environments, such as the weather in Hilo, may trigger a nail condition known as onychomycosis. In this condition, the fungus grows under the nails, and as a result, the nails become brittle and yellow. Treatment involves medication against the fungus.

Glands
Sweat Glands
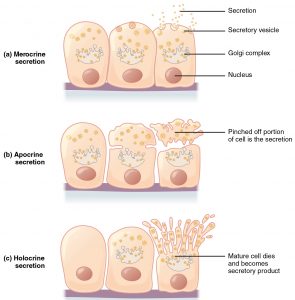
What does it mean to be cool? Our sweat glands (s) produce sweat (perspiration) to make us cool. The sweat gets to the skin surface either by traveling along the hair follicle or directly through the pores of the skin. The two types of sweat glands are eccrine and apocrine and they are divided by their differences in where and when they release sweat as well as the composition of their sweat.
 |
 |
| Gland Secretions | Layers of Skin with Sweat Glands |
Fig. 5.16: Sweat Glands Section of skin showing eccrine (merocrine) and apocrine sweat glands
You have a lot more s than s because eccrine sweat glands play a major role in creating the fluid on your skin surface that evaporates to lower your body temperature. This control of body temperature is a homeostatic mechanism called thermoregulation. Eccrine sweat glands also produce sweat when you are nervous, regardless of your body temperature, but their primary role is to keep you cool. These glands are all over your skin and most abundant on your forehead, palms, and soles. They are coiled structures deep in the dermis with their excretory duct opening as a pore of the skin. The sweat from eccrine sweat glands is mostly water with salt (sodium chloride), a very slight amount of metabolic waste, and dermcidin, a protein that can fight off harmful bacteria or a fungus.
You can thank your apocrine sweat glands for body odor. Or can you? It is not actually the sweat from these glands that creates that musky smell. It is the metabolism of apocrine sweat molecules by the skin’s normal bacteria that causes the odor. The sweat from apocrine sweat glands is different from that of eccrine sweat glands in that it also has fats and proteins. Apocrine sweat glands are coiled similar to eccrine sweat glands but they release their contents into the hair follicle. They are located in the armpits, groin, skin around the nipples, and in the beard region. Have you ever wondered why you didn’t have body odor until after puberty? It is because apocrine sweat glands are mostly inactive until then. If you put this information together with the change in hair pattern that occurs during puberty, it makes sense because the hair in the armpits, groin, chest, and beard changes from vellus hairs to terminal hairs during puberty. This connection to puberty goes further in that apocrine sweat glands release their sweat during sexual arousal. Similar to eccrine sweat glands, apocrine sweat glands also release sweat during strong emotions or nervousness.
The name, apocrine sweat gland, is unfortunate because an apocrine gland by definition pinches off part of itself in the process of releasing its product (see tissue chapter). However, apocrine sweat glands do not release their contents in the apocrine gland manner. They release sweat through exocytosis, as do eccrine sweat glands, which makes apocrine sweat glands a type of merocrine gland, not a type of apocrine gland. Maybe you will be the scientist who figures out something new one day and we will be adding notes to reference books because you discovered a new truth!
Sebaceous Glands
Oil glands (sebaceous glands) mostly release their contents into the hair follicle. The exceptions are the eyelids, labia minora, glans penis, and lips. In each of those locations, the oil is released through a pore in the skin. You have oil glands everywhere except your palms and soles, which should not surprise you since you don’t have hair there either. The oil released is called and it keeps the hair and skin from drying.
Ceruminous Glands
Inside your ear, you have modified sweat glands that produce a waxy substance. These ceruminous glands (“cer-” =wax) in combination with the sebaceous glands produce earwax, a yellow substance that is also called cerumen. Earwax helps to keep pathogens out of your ear by providing waterproofing and stickiness that catches things before they go deeper. Using cotton swabs in the ear canal can press the ear wax into the ear, impacting it and cause discomfort and difficulty hearing. It is treated by healthcare providers using irrigation (strongly focused spray of water) or removal with an instrument that can pull it out.
![]() Retrieval Practice
Retrieval Practice
Review all the layers of the skin and also the glands found in the skin. Put away your book and your notes and make a rough sketch of a cross-section of the skin. Include labels of all layers and types of glands. Go back to Figure 1 and correct any errors on your sketch and add in any missing items or layers. There is a lot of detail and new words so pat yourself on the back for making progress learning about the skin.
5.4 Skin Diseases, Disorders and Injuries
![]() 5.4 Learning Outcome
5.4 Learning Outcome
- Describe the skin disorders and injuries
Eczema
(atopic dermatitis) is an inflammatory disorder that manifests as dry, itchy patches of skin that resemble rashes. The small raised bumps associated with an eczema rash may leak fluid and crust over when scratched, resulting in raw, sensitive or thickened, cracked scaly skin. In severe cases, the swelling and cracking of the skin can result in bleeding and infection. There is no cure for atopic dermatitis and treatment consists of palliative care. Symptoms are usually managed with moisturizers, corticosteroid creams, and, based on recent research, immunosuppressants.

Fig. 5.17: Eczema Progression
![]() Cultural Connection: Kukui Tree
Cultural Connection: Kukui Tree
Pupuhi kukui — malino ke kai.
Spewed kukui nuts — calm sea.
To calm the water, fishermen chew kukui nuts and spew them. It has the same meaning as, “Pour oil on troubled waters.”
The Hawaiian practice of Lāʻau Lapaʻau incorporates the use of oil derived from the nut of the kukui tree (Aleurites moluccana). Introduced to Hawaiʻi more than 1500 years ago by Polynesian voyagers, the kukui tree and its derivatives (the flowers, fruits, nuts, bark, and leaves) are a commonly used laʻau (a plant used for medicinal purposes). Native Hawaiians often use the kukui nut for skin healing. Kukui nuts are pounded and/or roasted, and the oil, on its own or mixed with other plants can be applied topically to the outer layer of the skin to help remedy irritation associated with skin ailments such as eczema and related puhoʻaʻai (infectious sores). In addition to medicinal uses, the kukui tree is highly valued and is regarded as a symbol of enlightenment, protection, and peace.
 |
 |
| Kukui Tree | Kukui Nut |
How to make kukui nut oil:
Burns
A major cause of accidental death are burns. A burn results when the skin is damaged by intense heat, radiation, electricity, or chemicals. The damage results in the death of skin cells, which can lead to a massive loss of fluid. Dehydration, electrolyte imbalance, and renal and circulatory failure follow, which can be fatal. Burn patients are treated with intravenous fluids to offset dehydration, as well as intravenous nutrients that enable the body to repair tissues and replace lost proteins. Another serious threat to the lives of burn patients is infection. Burned skin is extremely susceptible to bacteria and other pathogens, due to the loss of protection by intact layers of skin.
Burns are sometimes measured in terms of the size of the total surface area affected. This is referred to as the “rule of nines,” which associates specific anatomical areas with a percentage that is a factor of nine. See burn figure 5.18. Burns are also classified by the degree of their severity. A first-degree burn is a superficial burn that affects only the epidermis. Mild sunburn is an example of this type of burn. Although the skin may be painful and swollen, these burns typically heal on their own within a few days. Mild sunburn fits into the category of a first-degree burn. A goes deeper and affects both the epidermis and a portion of the dermis. These burns result in swelling and painful blistering of the skin. It is important to keep the burn site clean and sterile to prevent infection. If this is done, the burn will heal within several weeks.
A fully extends into the epidermis and dermis, destroying the tissue and affecting the nerve endings and sensory function. These are serious burns that may appear white, red, or black; they require medical attention and will heal slowly without it. A is even more severe, affecting the underlying muscle and bone. Third- and fourth-degree burns can be caused by fire or exposure to really hot water. Oddly, third and fourth-degree burns are usually not as painful because the nerve endings themselves are damaged. Full-thickness burns cannot be repaired by the body, because the local tissues used for repair are damaged and require excision (debridement), or amputation in severe cases, followed by grafting of the skin from an unaffected part of the body, or from skin grown in tissue culture for grafting purposes.
The severity of a burn is calculated by considering the following aspects: degree of the burn, location and size of the burn, and the age of the person. To have an idea of the surface area of a burn, health professionals use the rule of nines, which implies that most regions of our bodies account for some factor of 9% of the total area related to the body surface. This determination is relevant when deciding how much fluids are needed to be replaced.

Fig. 5.18 Calculating the Size of a Burn The size of a burn will guide decisions made about the need for specialized treatment. Specific parts of the body are associated with a percentage of the body area.
Bedsores
Skin and its underlying tissue can be affected by excessive pressure. One example of this is called a . Bedsores, also called decubitus ulcers, are caused by constant, long-term, unrelieved pressure on certain body parts that are bony, reducing blood flow to the area and leading to necrosis (tissue death). Bedsores are most common in elderly patients who have debilitating conditions that cause them to be immobile. Most hospitals and long-term care facilities have the practice of turning the patients every few hours to prevent the incidence of bedsores. If left untreated by the removal of necrotized tissue, bedsores can be fatal if they become infected.
Stretch Marks
The skin can also be affected by pressure associated with rapid growth. A results when the dermis is stretched beyond its limits of elasticity, as the skin stretches to accommodate the excess pressure. Stretch marks usually accompany rapid weight gain during puberty and pregnancy. They initially have a reddish hue, but lighten over time. Other than for cosmetic reasons, treatment of stretch marks is not required. They occur most commonly over the hips and abdomen.

Chapter Summary

Key Terms
albinism
genetic disorder that affects the skin, in which there is no melanin production
apocrine sweat gland
type of sweat gland that is associated with hair follicles in the armpits and genital regions
arrector pili
smooth muscle that is activated in response to external stimuli that pull on hair follicles and make the hair “stand up”
basal cell
type of stem cell found in the stratum basale and in the hair matrix that continually undergoes cell division, producing the keratinocytes of the epidermis
basal cell carcinoma
cancer that originates from basal cells in the epidermis of the skin
bedsore
sore on the skin that develops when regions of the body start necrotizing due to constant pressure and lack of blood supply; also called decubitis ulcers
callus
thickened area of skin that arises due to constant abrasion
cortex
in hair, the second or middle layer of keratinocytes originating from the hair matrix, as seen in a cross-section of the hair bulb
cuticle
in hair, the outermost layer of keratinocytes originating from the hair matrix, as seen in a cross-section of the hair bulb
dermal papilla
(plural = dermal papillae) extension of the papillary layer of the dermis that increases surface contact between the epidermis and dermis
dermis
layer of skin between the epidermis and hypodermis, composed mainly of connective tissue and containing blood vessels, hair follicles, sweat glands, and other structures
desmosome
structure that forms an impermeable junction between cells
eccrine sweat gland
type of sweat gland that is common throughout the skin surface; it produces a hypotonic sweat for thermoregulation
eczema
skin condition due to an allergic reaction, which resembles a rash
elastin fibers
fibers made of the protein elastin that increase the elasticity of the dermis
eleiden
clear protein-bound lipid found in the stratum lucidum that is derived from keratohyalin and helps to prevent water loss
epidermis
outermost tissue layer of the skin
eponychium
nail fold that meets the proximal end of the nail body, also called the cuticle
fourth-degree burn
burn in which full thickness of the skin and underlying muscle and bone is damaged
hair
keratinous filament growing out of the epidermis
hair bulb
structure at the base of the hair root that surrounds the dermal papilla
hair follicle
cavity or sac from which hair originates
hair matrix
layer of basal cells from which a strand of hair grows
hair root
part of hair that is below the epidermis anchored to the follicle
hair shaft
part of hair that is above the epidermis but is not anchored to the follicle
hypodermis
connective tissue connecting the integument to the underlying bone and muscle
hyponychium
thickened layer of stratum corneum that lies below the free edge of the nail
integumentary system
skin and its accessory structures
keratin
type of structural protein that gives skin, hair, and nails its hard, water-resistant properties
keratinocyte
cell that produces keratin and is the most predominant type of cell found in the epidermis
keratohyalin
granulated protein found in the stratum granulosum
Langerhans cell
specialized dendritic cell found in the stratum spinosum that functions as a macrophage
lunula
basal part of the nail body that consists of a crescent-shaped layer of thick epithelium
medulla
in hair, the innermost layer of keratinocytes originating from the hair matrix
Meissner corpuscle
(also, tactile corpuscle) receptor in the skin that responds to light touch
melanin
pigment that determines the color of hair and skin
melanocyte
cell found in the stratum basale of the epidermis that produces the pigment melanin
melanoma
type of skin cancer that originates from the melanocytes of the skin
melanosome
intercellular vesicle that transfers melanin from melanocytes into keratinocytes of the epidermis
Merkel cell
receptor cell in the stratum basale of the epidermis that responds to the sense of touch
nail bed
layer of epidermis upon which the nail body forms
nail body
main keratinous plate that forms the nail
nail cuticle
fold of epithelium that extends over the nail bed, also called the eponychium
nail fold
fold of epithelium at that extend over the sides of the nail body, holding it in place
nail root
part of the nail that is lodged deep in the epidermis from which the nail grows
Pacinian corpuscle
(also, lamellated corpuscle) receptor in the skin that responds to vibration
papillary layer
superficial layer of the dermis, made of loose, areolar connective tissue
reticular layer
deeper layer of the dermis; it has a reticulated appearance due to the presence of abundant collagen and elastin fibers
scar
collagen-rich skin formed after the process of wound healing that is different from normal skin
sebaceous gland
type of oil gland found in the dermis all over the body and helps to lubricate and waterproof the skin and hair by secreting sebum
sebum
oily substance that is composed of a mixture of lipids that lubricates the skin and hair
second-degree burn
partial-thickness burn that injures the epidermis and a portion of the dermis
stratum basale
deepest layer of the epidermis, made of epidermal stem cells
stratum corneum
most superficial layer of the epidermis
stratum granulosum
layer of the epidermis superficial to the stratum spinosum
stratum lucidum
layer of the epidermis between the stratum granulosum and stratum corneum, found only in thick skin covering the palms, soles of the feet, and digits
stratum spinosum
layer of the epidermis superficial to the stratum basale, characterized by the presence of desmosomes
stretch mark
mark formed on the skin due to a sudden growth spurt and expansion of the dermis beyond its elastic limits
sudoriferous gland
sweat gland
third-degree burn
burn that penetrates and destroys the full thickness of the skin (epidermis and dermis)
vitamin D
compound that aids absorption of calcium and phosphates in the intestine to improve bone health
vitiligo
skin condition in which melanocytes in certain areas lose the ability to produce melanin, possibly due an autoimmune reaction that leads to loss of color in patches
Sources
- Some sections were modified from OpenStax Anatomy and Physiology (http://OpenStax.org/details/books/anatomy-and-physiology)
- Figure 1: “Structure of mammalian skin and the layers typically present in parchment” by Sean P Doherty via Wikimedia Commons/CC BY-SA 4.0
- Figure 2: Left: “Layers of Epidermis” By OpenStax College via Wikimedia Commons/CC BY 3.0, Right: “Epidermis layers” By Mikael Häggström, based on work by Wbensmith via Wikimedia Commons/CC BY-SA 3.0
- Ukulele picture: https://commons.wikimedia.org/w/index.php?search=ukulele&title=Special:MediaSearch&go=Go&type=image
- Young, Ryan & Cruz, Luis & Brown, Amy. (2005). Indigenous Hawaiian Nonmedical and Medical Use of the Kukui Tree. Journal of alternative and complementary medicine (New York, N.Y.). 11. 397-400. 10.1089/acm.2005.11.397.
- http://www.canoeplants.com/kukui.html
- Look M.A., Yamauchi K.B., Trask-Batti M.K., Werner K.W., & Lee W.K. (2013). Guide to Selected Plants of the Mala Lāʻau Lapaʻau at JABSOM. Honolulu, HI: Department of Native Hawaiian Health, John A. Burns School of Medicine, University of Hawaiʻi at Mānoa
- Skin Stories, PBS Hawai’i: https://www.pbs.org/skinstories/history/index.html
Media Attributions
- olelo_noeau
- Pixabay beach-1853540_1920 © Image by Pexels from Pixabay is licensed under a Public Domain license
- Wiki Cross Section Skin 1272px-Skin-_epidermis_and_dermis © National Cancer Institute is licensed under a Public Domain license
- Skin Layers © Sean P Doherty is licensed under a CC BY-SA (Attribution ShareAlike) license
- Layers Epidermis
- Wiki Epidermal_layers © Mikael Häggström is licensed under a CC BY-SA (Attribution ShareAlike) license
- Wiki Ukulele_F_Chord © Alan Levine is licensed under a CC BY-SA (Attribution ShareAlike) license
- Wiki 512px-Uke_sizes_and_scale_lengths © LardyFatBoy is licensed under a CC BY-SA (Attribution ShareAlike) license
- Wiki Nursing_and_Public_Health_students_at_University_of_Hawaii_provide_free_blood_pressure_screenings_for_the_Global_Day_of_Action_(15003396243) © Article 25 Flickr is licensed under a CC BY-SA (Attribution ShareAlike) license
- Wiki Albinisitic_man_portrait © Karl Neilson is licensed under a CC BY-SA (Attribution ShareAlike) license
- Wiki Vitiligo Ferguson_Day_7,_Picture_8_(cropped) © Loavesofbread is licensed under a CC BY-SA (Attribution ShareAlike) license
- Wiki 1440px-UV_and_Vis_Sunscreen © Spigget is licensed under a CC BY-SA (Attribution ShareAlike) license
- Wiki Basal_cell_carcinoma © John Hendrix is licensed under a Public Domain license
- Wiki ABCDE Melanoma 810px-Melanoma_vs_normal_mole_ABCD_rule_NCI_Visuals_Online © Stevenfruitsmaak / NIH is licensed under a Public Domain license
- Med Libre skin-layers1 cc by sa © LibreTexts is licensed under a CC BY-SA (Attribution ShareAlike) license
- Wiki Epidermis,_papillary_dermis_and_reticular_dermis © Original by Kilbad. Derivative by Mikael Häggström, M.D. is licensed under a CC BY (Attribution) license
- Wiki Fingerprint_-_Central_Pocket_Loop_Whorl © Saurabh R. Patil is licensed under a CC BY-SA (Attribution ShareAlike) license
- Wiki 1620px-Fingerprint_detail_on_male_finger_in_Třebíč,_Třebíč_District © Frettie is licensed under a CC BY (Attribution) license
- Wiki Jason_Momoa_by_Gage_Skidmore © Gage Skidmore is licensed under a CC BY-SA (Attribution ShareAlike) license
- Wiki Moko Tattoo Hon_Nanaia_Mahuta © New Zealand Labour Party is licensed under a CC BY-SA (Attribution ShareAlike) license
- Wiki Samoan_Malu © RunningToddler - Bits & Bytes is licensed under a CC BY-SA (Attribution ShareAlike) license
- Tinglayan Area © Mawg64 is licensed under a CC BY-SA (Attribution ShareAlike) license
- Wiki YoungNoni under 1m © Travis.Thurston is licensed under a CC BY-SA (Attribution ShareAlike) license
- Wiki Noni_fruit_(Morinda_citrifolia) 8k © Wilfredor is licensed under a CC0 (Creative Commons Zero) license
- Wiki 1082px-Goosebumps_in_cat © SKsiddhartthan is licensed under a CC BY-SA (Attribution ShareAlike) license
- Piloerection (Chicken Skin) Goosebumps © Ildar Sagdejev (Specious) is licensed under a CC BY-SA (Attribution ShareAlike) license
- Wiki Blausen_0406_FingerNailAnatomy © BruceBlaus is licensed under a CC BY (Attribution) license
- Wiki 1102px-Oncymycosis © James Heilman, MD is licensed under a CC BY-SA (Attribution ShareAlike) license
- Glandular Secretion © Openstax is licensed under a CC BY (Attribution) license
- Layers of Skin with Sweat Glands 9k © Openstax is licensed under a CC BY (Attribution) license
- Wiki Eczema_Progression © BruceBlaus is licensed under a CC BY-SA (Attribution ShareAlike) license
- Wiki Kukui Aleurites_moluccanus © Shyamal is licensed under a CC BY-SA (Attribution ShareAlike) license
- Wiki Kukui Kemiri_atau_damo © Andri Kesenja 01 is licensed under a CC BY-SA (Attribution ShareAlike) license
- Calculating Burn Size © Openstax is licensed under a CC BY (Attribution) license
- Honu_‘Iwalani Clayton_CCBY_2022 10 30 © ‘Iwalani Clayton is licensed under a CC BY (Attribution) license
- divider_maile
Skin and its accessory structures.
Keratinous filament growing out of the epidermis.
Outermost tissue layer of the skin.
Cell that produces keratin and is the most predominant type of cell found in the epidermis.
Cell found in the stratum basale of the epidermis that produces the pigment melanin.
Receptor cell in the stratum basale of the epidermis that responds to the sense of touch.
Specialized dendritic cell found in the stratum spinosum that functions as a macrophage.
Deepest layer of the epidermis, made of epidermal stem cells.
Most superficial layer of the epidermis.
Type of structural protein that gives skin, hair, and nails its hard, water-resistant properties.
Layer of the epidermis superficial to the stratum spinosum.
Layer of the epidermis between the stratum granulosum and stratum corneum, found only in thick skin covering the palms, soles of the feet, and digits.
Clear protein-bound lipid found in the stratum lucidum that is derived from keratohyalin and helps to prevent water loss.
Layer of the epidermis superficial to the stratum basale, characterized by the presence of desmosomes.
Granulated protein found in the stratum granulosum.
Structure that forms an impermeable junction between cells.
Type of stem cell found in the stratum basale and in the hair matrix that continually undergoes cell division, producing the keratinocytes of the epidermis.
Layer of skin between the epidermis and hypodermis, composed mainly of connective tissue and containing blood vessels, hair follicles, sweat glands, and other structures.
Thickened area of skin that arises due to constant abrasion.
Pigment that determines the color of hair and skin.
Genetic disorder that affects the skin, in which there is no melanin production.
Skin condition in which melanocytes in certain areas lose the ability to produce melanin, possibly due an autoimmune reaction that leads to loss of color in patches.
Intercellular vesicle that transfers melanin from melanocytes into keratinocytes of the epidermis.
Cancer that originates from basal cells in the epidermis of the skin.
Type of skin cancer that originates from the melanocytes of the skin.
Compound that aids absorption of calcium and phosphates in the intestine to improve bone health.
Cavity or sac from which hair originates.
Type of oil gland found in the dermis all over the body and helps to lubricate and waterproof the skin and hair by secreting sebum.
Superficial layer of the dermis, made of loose, areolar connective tissue.
Deeper layer of the dermis; it has a reticulated appearance due to the presence of abundant collagen and elastin fibers.
Fibers made of the protein elastin that increase the elasticity of the dermis.
(Plural = dermal papillae) extension of the papillary layer of the dermis that increases surface contact between the epidermis and dermis.
(Also, tactile corpuscle) receptor in the skin that responds to light touch.
Connective tissue connecting the integument to the underlying bone and muscle.
Collagen-rich skin formed after the process of wound healing that is different from normal skin.
(Also, lamellated corpuscle) receptor in the skin that responds to vibration.
Part of hair that is above the epidermis but is not anchored to the follicle.
Part of hair that is below the epidermis anchored to the follicle.
Structure at the base of the hair root that surrounds the dermal papilla.
Layer of basal cells from which a strand of hair grows.
In hair, the outermost layer of keratinocytes originating from the hair matrix, as seen in a cross-section of the hair bulb.
In hair, the second or middle layer of keratinocytes originating from the hair matrix, as seen in a cross-section of the hair bulb.
in hair, the innermost layer of keratinocytes originating from the hair matrix
Smooth muscle that is activated in response to external stimuli that pull on hair follicles and make the hair “stand up.”
Layer of epidermis upon which the nail body forms.
Main keratinous plate that forms the nail.
Part of the nail that is lodged deep in the epidermis from which the nail grows.
Fold of epithelium at that extend over the sides of the nail body, holding it in place.
Fold of epithelium that extends over the nail bed, also called the eponychium.
Nail fold that meets the proximal end of the nail body, also called the cuticle.
Basal part of the nail body that consists of a crescent-shaped layer of thick epithelium.
Thickened layer of stratum corneum that lies below the free edge of the nail.
Sweat gland.
Type of sweat gland that is common throughout the skin surface; it produces a hypotonic sweat for thermoregulation.
Type of sweat gland that is associated with hair follicles in the armpits and genital regions.
Oily substance that is composed of a mixture of lipids that lubricates the skin and hair.
Skin condition due to an allergic reaction, which resembles a rash.
Partial-thickness burn that injures the epidermis and a portion of the dermis.
Burn that penetrates and destroys the full thickness of the skin (epidermis and dermis).
Burn in which full thickness of the skin and underlying muscle and bone is damaged.
Sore on the skin that develops when regions of the body start necrotizing due to constant pressure and lack of blood supply; also called decubitis ulcers.
Mark formed on the skin due to a sudden growth spurt and expansion of the dermis beyond its elastic limits.
